Last Updated: October 30, 2025
Introduction to OTC Deficiency
Deficiencies in each of the enzymes of the urea cycle have been identified. Collectively, these enzyme deficiencies lead to a family of disorders referred to as the urea cycle disorders (UCD). The most dramatic presentation of UCD symptoms occurs in neonates between 24 and 48 hours after birth (sometimes symptoms are delayed for several days). Afflicted infants exhibit progressively deteriorating symptoms due to the elevated ammonium levels.
Deficiency in ornithine transcarbamylase (OTC; also called ornithine carbamoyltransferase) is the most commonly occurring UCD with a frequency of approximately 1 case in every 14,000 live births. OTC deficiency is inherited as an X-linked disorder, classically referred to as X-linked recessive.
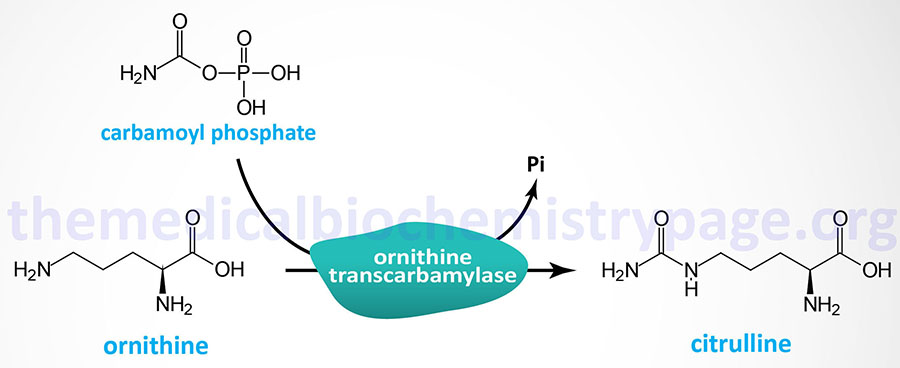
Ornithine transcarbamylase (OTC) catalyzes the condensation of carbamoyl phosphate with ornithine forming citrulline. Like the urea cycle reaction catalyzed by carbamoyl phosphate synthetase 1 (CPS1), the OTC reaction takes place within the mitochondria.
Molecular Biology of OTC
Ornithine transcarbamylase is encoded by the OTC gene. The OTC gene is located on the X chromosome (Xp11.4), spans more than 85 kb, and is comprised of 10 exons that generate two alternatively spliced mRNAs, both of which encode the same precursor protein of 354 amino acids.
There have been over 158 different mutant alleles of the OTC gene identified in OTCD. In males, 98% receive a mutant allele from their mothers, whereas, in females, 9%–10% of mutant OTC carriers acquired their mutation sporadically.
Clinical Features of OTC Deficiency
OTCD is, like the other neonatal onset forms of UCDs, most severe when presenting in newborn infants. As with each of the four neonatal onset UCDs, OTCD is characterized by the accumulation of ammonia and glutamine with clinical manifestations appearing in full-term infants with no prior obstetric risk factors.
The classic symptoms appear between 24hrs and 48hrs after birth (but not prior to 24hrs) and include convulsions, hyperventilation, ataxia, hypothermia, lethargy, vomiting and poor feeding. If left untreated the hyperammonemia with result in coma and death. The severe effects of hyperammonemia are described in the Nitrogen Metabolism and Urea Cycle page. Even though sepsis is a rare event in a normal term infant with no prior obstetric complications, this disorder is misdiagnosed in almost half of neonatal UCD cases.
Initial laboratory findings will include respiratory alkalosis which is the earliest objective indication of encephalopathy. The encephalopathy will progress to the point where mechanical ventilation is required. Another routine laboratory finding is reduced serum (blood) urea nitrogen (BUN) which may be as low as 1mg/dl (normal for newborns is 3–12mg/dl). If plasma ammonia levels are not measured the infants’ death will be attributed to sepsis, intracranial hemorrhage, or some other disorder that would normally be associated with a pre-term delivery.
Treatment of OTC Deficiency
OTCD patients are treated in much the same ways as for other neonatal UCDs in that protein intake must me highly regulated and the hyperammonemia must be controlled. Hemodialysis is the only effective means to rapidly lower serum ammonia levels in these patients. Acute episodes of hyperammonemia can be treated with intravenous administration of Ammunol® and with oral Buphenyl® for chronic adjunctive therapy of hyperammonemia. The mechanism of action of these compounds is detailed in the Urea Cycle Disorders: Overview page.
OTCD patients are treated with a strict dietary regimen that includes 0.7g/kg/day of protein and 0.7g/kg/day of an essential amino acid mixture. The diet is also supplemented with citrulline to serve as a source of arginine. As development proceeds and the need for protein declines it is necessary to adjust the dietary intake of protein accordingly.
