Last updated: June 6, 2025
Introduction to Organic Acidurias
Organic aciduria (OAD) refers to a biochemically defined group of inherited metabolic diseases resulting from failure to metabolize various organic acids. The OAD can result from mutations in genes encoding enzymes of fatty acid metabolism, enzymes of amino acid metabolism, and enzymes involved in several other metabolic pathways such as the TCA cycle. Evidence strongly indicates that the progression of pathology in most OAD is best explained by mitochondrial dysfunction.
The term organic aciduria originated from the measurement of organic acids, nonamino mono-, di- or tricarboxylic acids, in the urine. In addition to the urine, these organic acids accumulate in the blood (organic acidemias) and the cerebrospinal fluid (CSF). In the majority of OAD the organic acid accumulates due to deficiency in the mitochondrial catabolism of various CoA-activated carbonic acids such as propionyl-CoA, methylmalonyl-CoA, isovaleryl-CoA, and glutaryl-CoA.
In several situations, patients with an OAD are found to develop cerebral neoplasms such as in L-2-hydroxyglutaric aciduria (L2HGA) and in glutaric aciduria type 1. In addition, hepatic cancers have been found to be associated with some of the methylmalonic acidemias.
Alkaptonuria
Alkaptonuria is a rare autosomal recessive disorder caused by defects in the gene encoding an enzyme, homogentisic acid oxidase, involved in the catabolism of phenylalanine and tyrosine. As a consequence of this gene defect the catabolism of these two amino acids is inhibited and the intermediate homogentisic acid is excreted in the urine.
The details of alkaptonuria are covered in the Alkaptonuria page.
Maple Syrup Urine Disease
Maple syrup urine disease (MSUD), also called branched-chain aminoaciduria, is so called because the urine of affected individuals smells like maple syrup or burnt sugar. MSUD is an autosomal recessive disorder that results from a deficiency in the enzyme, branched-chain α-keto acid dehydrogenase (BCKD), that is involved in the catabolism of the branched-chain amino acids (BCAA), leucine, isoleucine, and valine. A deficiency in BCKD leads to an accumulation of those three amino acids and their corresponding branched-chain α-keto acids (BCKA). MSUD is associated with a worldwide frequency of approximately 1 in 185,000 persons. In certain inbred populations such as the Old Order Mennonites the incidence of MSUD is extremely high on the order of 1 in every 175 births.
The details of MSUD are discussed in the Maple Syrup Urine Disease (MSUD) page.
Isovaleric Acidemia
Isovaleric acidemia (IVA) is an autosomal recessive disorder that is a member of the family of disorders referred to as the organic acidemias. Indeed, IVA was the first inborn error of metabolism to be characterized as an organic acidemia. Isovaleric acid is an intermediate in the catabolism of the branch-chain amino acid, leucine that accumulates as a result of mutations in the gene encoding isovaleryl-CoA dehydrogenase (IVD).
The details of isovaleric acidemia are covered in the Isovaleric Acidemia page.
Propionic Aciduria
Propionic acidemia is a member of the family of disorders termed organic acidemias. Propionic acidemia is an autosomal recessive disorder that results from mutations in either of the two genes encoding the subunits of the mitochondrial enzyme, propionyl-CoA carboxylase (PCC). The incidence of propionic acidemia is approximately 1:100,000.
Propionic acidemia is a clinically heterogeneous disorder divided into a neonatal lethal form and a late-onset form that appears in older children or adults. The neonatal-onset form manifests shortly after birth in an otherwise healthy infant. The neonatal-onset form of the disease is the more common form of propionic acidemia.
The details of propionic acidemia are covered in the Propionic Acidemia page.
Glutaric Aciduria Type 1
Glutaric aciduria type 1 (also known as glutaric acidemia type 1) is an autosomal recessive disorder of amino acid metabolism. The disorder is the result of defects in the mitochondrial matrix enzyme, glutaryl-CoA dehydrogenase (GCDH). Glutaryl-CoA dehydrogenase is a member of the acyl-CoA dehydrogenase family of enzymes that includes those involved in mitochondrial β-oxidation of fatty acids and as such the enzyme is also known as acyl-CoA dehydrogenase 5 (ACAD5). Glutaryl-CoA dehydrogenase catalyzes the conversion of glutaryl-CoA to crotonyl-CoA in the catabolism of the amino acids lysine, tryptophan, and hydroxylysine.
The details of glutaric aciduria type 1 are covered in the Glutaric Aciduria Type 1 page.
Methylmalonic Acidurias/Acidemias
The methylmalonic acidemias (methylmalonic acidurias) represent a family of disorders that have, in common, the elevation of methylmalonic acid in the blood (emia) and urine (uria). Some of the methylmalonic acidemias also include the presence of homocystinuria and are referred to as combined methylmalonic acidemia and homocystinuria.
The details of the methylmalonic acidurias are covered in the Methylmalonic Acidemias/Acidurias page.
2-Hydroxyglutaric Acidurias
The 2-hydroxyglutaric acidurias represents a family of related metabolic disorders that are due to the accumulation of one or the other, or both, of the stereoisomers of 2-hydroxyglutarate (2-HG), namely D-2-hydroxyglutaric acid and L-2-hydroxyglutaric acid in the blood, cerebrospinal fluid (CSF), and the urine. The accumulation of these compounds primarily results from defects in D-2-hydroxyglutarate dehydrogenase or L-2-hydroxyglutarate dehydrogenase or due to defects in both enzymes. Both enzymes are localized to the mitochondria.
The primary 2-hydroxyglutaric aciduria that results from accumulation of D-2-hydroxyglutaric acid is designated the D2HGA1. The 2-hydroxyglutaric aciduria that results from accumulation of L-2-hydroxyglutaric acid is designated L2HGA. When both D- and L-2-hydroxyglutarate accumulation is the cause of disease it is designated D2L2AD. An additional form of 2-hydroxglutaric aciduria, specifically D-2-hydroxyglutaric aciduria type 2 (D2HGA2), is the result of gain-of-function mutations in the IDH2 (isocitrate dehydrogenase 2) gene.
As indicated, 2-hydroxyglutarate (2-HG) exists in two stereoisomeric configurations, D-2-hydroxyglutarate and L-2-hydroxyglutarate. The normal pathways for the synthesis of 2-HG utilize 2-oxoglutarate (α-ketoglutarate) or γ-hydroxybutyrate (GHB) as the substrate. Mitochondrial malate dehydrogenase (MDH2) converts 2-oxoglutarate to 2-HG while alcohol dehydrogenase iron containing 1 (encoded by the ADHFE1 gene) converts GHB to 2-HG and succinic semialdehyde (SSA). The ADHFE1 encoded enzyme is also known as hydroxyacid-oxoacid transhydrogenase (HOT).
The catabolism of 2-HG is catalyzed by stereospecific dehydrogenases, D-2-hydroxyglutarate dehydrogenase and L-2-hydroxyglutarate dehydrogenase. The product of the 2-hydroglutarate dehydrogenases is 2-oxoglutarate (α-ketoglutarate).
D-2-hydroxyglutarate dehydrogenase is encoded by the D2HGDH gene. The D2HGDH gene is located on chromosome 2q37.3 and is composed of 18 exons that generate three alternatively spliced mRNAs, each of which encode distinct precursor proteins.
L-2-hydroxyglutarate dehydrogenase is an FAD-dependent enzyme encoded by the L2HGDH gene. The L2HGDH gene is located on chromosome 14q21.3 and is composed of 15 exons that encode a 463 amino acid precursor protein.
The clinical manifestations of D2HGA1 and D2HGA2 are very similar but the age of onset is different. D2HGA1 usually manifests in the first six months of life whereas D2HGA2 manifests with an average age of onset of two years. The cardinal clinical manifestations for both D2HGA1 and D2HGA2 are developmental delay, hypotonia, and seizures. Seizures occur with a higher frequency in D2HGA2 compared to D2HGA1. All D2HGA2 patients that have been identified exhibited developmental delay and to a more severe degree than that seen in D2HGA1 patients. The life expectancy for D2HGA1 patients remains undefined while that for D2HGA2 patients is from several months of diagnosis to adulthood.
The cardinal clinical manifestations of L2HGA include an insidious onset of disease beginning in childhood and includes developmental delay, epilepsy, and cerebellar ataxia. Nearly all L2HGA patients will display delayed mental and motor development. Roughly 70% of L2HGA patients will exhibit epilepsy and cerebellar dysfunction. Hypotonia is most prevalent in the earlier stages of the disease while spasticity is seen in the latter stages of disease. The progression of pathology in L2HGA is slow which means some patients may not be correctly diagnosed until adolescence of adulthood. MRI studies in several L2HGA patients found highly characteristic abnormalities of the subcortical cerebral white matter dentate nucleus,
globus pallidus, putamen, and caudate nucleus.
Very few cases of combined of D,L-2-hydroxyglutaric aciduria (D2L2AD) have been described. The biochemical characterization of D2L2AD includes a finding of moderately elevated levels of both D-2-HG and L-2-HG in urine, mild increases of both metabolites in the blood, and a very slight elevation of D-2-HG in CSF with normal CSF levels of L-2-HG. In the patients that have been clearly diagnosed with D2L2AD the consistent clinical manifestations include severe neonatal epileptic encephalopathy, often accompanied by respiratory insufficiency requiring artificial ventilation. When MRI was used to examine the brains of D2L2AD patients it was found that all showed enlarged ventricles, subependymal pseudocysts, and delayed gyration and myelination.
3-Hydroxy-3-Methylglutaric Aciduria
Mutations in the HMGCL gene, that encodes 3-hydroxy-3-methylglutaryl-CoA lyase (HMG-CoA lyase), result in a disorder referred to as 3-hydroxy-3-methylglutaric aciduria. Inheritance of 3-hydroxy-3-methylglutaric aciduria occurs as an autosomal recessive disorder. The function of 3-hydroxy-3-methylglutaryl-CoA lyase is to catalyze the hydrolysis of 3-hydroxy-3-methylglutaryl-CoA to acetyl-CoA and acetoacetate during the catabolism of leucine.
Since the enzyme encoded by the HMGCL gene is also involved in ketone body synthesis, mutations in the HMGCL gene also result in defects in ketone synthesis. The reduced capacity to synthesize the ketones, acetoacetate and β-hydroxybutyrate, results in inefficient energy production by the brain during periods of fasting. Reduced HMG-CoA lyase activity is associated with episodes of hypoglycemia and metabolic acidosis.
The HMGCL gene is located on chromosome 1p36.11 and is composed of 9 exons that generate two alternatively spliced mRNAs. These two mRNAs encode mitochondrially localized proteins that are synthesized as precursor proteins of 325 amino acids (isoform 1) and 254 amino acids (isoform 2).
Characteristic findings in patients with mutations in the HMGCL gene are accumulation of leucine metabolites, 3-hydroxy-3-methylglutaric acid, 3-methylglutaconic acid, 3-methylglutaric acid, and 3-hydroxyisovaleric acid. HMG-CoA lyase deficiency is treatable by diet, particularly leucine restriction, and avoidance of prolonged fasting. Supplementary glucose is administered to prevent hypoglycemia. Without prompt and proper therapeutic intervention, death occurs early in life.
3-Methylcrotonylglycinuria
3-Methylcrotonylglycinuria is a disorder of leucine catabolism that results from defects in either of the two subunits of the biotin-requiring enzyme, 3-methylcrotonyl-CoA carboxylase (3MCC). 3-Methylcrotonylglycinuria is also referred to as 3-methylcrotonyl-CoA carboxylase deficiency (3-MCCD). The function of 3-methylcrotonyl-CoA carboxylase is to catalyze the carboxylation of 3-methylcrotonyl-CoA to 3-methylglutaconyl-CoA during the catabolism of leucine. The 3-methylcrotonyl-CoA is the product of isovaleryl-CoA dehydrogenase which catalyzes the previous reaction in leucine catabolism.
As indicated, 3MCC is composed of two subunits in a heterododecameric configuration composed of six α-subunits and six β-subunits (α6β6). The activity of 3MCC is dependent on biotin. The α-subunit covalently binds biotin while the carboxyltransferase activity is encoded by the β-subunit. The structure of 3MCC and its dependence on biotin make it highly similar in structure and catalytic activity to propionyl-CoA carboxylase, PCC. The α-subunit of 3MCC is encoded by the MCCC1 gene and the β-subunit is encoded by the MCCC2 gene. Mutations in the MCCC1 gene cause 3-methylcrotonylglycinuria type I, while mutations in the MCCC2 gene cause 3-methylcrotonylglycinuria type II.
The MCCC1 gene is located on chromosome 3q27.1 and is composed of 23 exons that generate three alternatively spliced mRNAs, two of which are known to encode functional protein. MCCC1 isoform 1 is a precursor protein of 725 amino acids and isoform 2 is a precursor protein of 608 amino acids. Mutations in the MCC1 gene are the cause of 3-methylcrotonylglycinuria type I.
The MCCC2 gene is located on chromosome 5q13.2 and is composed of 19 exons that generate two alternatively spliced mRNAs encoding precursor proteins of 563 amino acids (isoform 1) and 525 amino acids (isoform 2).
Inheritance of 3-methylcrotonylglycinuria occurs in an autosomal recessive manner. The symptoms that result from defects in either of the two genes encoding 3MCC can range from benign to profound metabolic acidosis and early death. In the more severe forms of 3MCC deficiency, infants appear normal at birth but will develop symptoms during the first year of life or possibly not until early childhood. The characteristic features of the severe forms of 3MCC deficiency include difficulty feeding, recurrent episodes of vomiting and diarrhea, lethargy, and hypotonia. If left undiagnosed or untreated, 3MCC deficiency can lead to delayed development, seizures, coma, and ultimately death.
3-Methylglutaconic Aciduria, Type 1
During the catabolism of leucine, the 3-methylglutaconyl-CoA is converted to 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) via the action of the bifunctional enzyme, 3-methylglutaconyl-CoA hydratase. The 3-methylglutaconyl-CoA hydratase enzyme possesses both RNA-binding and hydratase activities accounting for the official name of the gene encoding this enzyme, AU RNA-binding methylglutaconyl-CoA hydratase (AUH). The AUH gene is located on chromosome 9q22.31 and is composed of 20 exons that generate five alternatively spliced mRNAs that collectively encode four distinct protein isoforms.
Mutations in the AUH gene result in the extremely rare autosomal recessive disorder referred to as 3-methylglutaconic aciduria, type 1 (MGCA1). To date less than 20 cases of MGCA1 have been identified. MGCA1 is associated with urinary excretion of 3-methylglutaconic acid and its derivatives, 3-methylglutaric acid and 3-hydroxyisovaleric acid. Patients with MGCA1 manifest with two main phenotypic presentations, a childhood presentation and an adult presentation. The childhood onset form of the disorder is associated with the nonspecific finding of psychomotor impairment. The adult onset form is associated with progressive neurodegeneration characterized by ataxia, spasticity, and sometimes dementia. The adult onset patients also develop white matter lesions in the brain.
There are nine identified forms of 3-methylglutaconic aciduria (MGCA1 to MGCA9), but only MGCA1 is associated with direct deficiency in leucine catabolism. MGCA1 can be distinguished from the other forms of MGCA because the levels of 3-methylglutaconic acid are highly elevated, whereas levels of methylglutaric acid are usually only slightly elevated, and there is a high level of 3-hydroxyisovaleric acid excretion which is not seen in the other forms of MGCA.
Holocarboxylase Synthetase Deficiency (Multiple Carboxylase Deficiency)
Holocarboxylase synthetase is the enzyme that attaches biotin to the biotin-dependent carboxylases, acetyl-CoA carboxylase (ACC), propionyl-CoA carboxylase (PCC), pyruvate carboxylase (PC), and 3-methylcrotonyl-CoA carboxylase (3MCC). Deficiency in holocarboxylase synthetase is an autosomal recessive disorder that results in deficiency in all four biotin-dependent carboxylases. For this reason the disorder is also known as multiple carboxylase deficiency.
Holocarboxylase synthetase is encoded by the HLCS gene. The HLCS gene is located on chromosome 21q22.13 and is composed of 19 exons that generate eight alternatively spliced mRNAs, seven of which encode the same 726 amino acid protein (isoform 1) and one which encodes a 873 amino acid protein (isoform 2). At least 35 different mutations in the HLCS gene have been found associated with holocarboxylase synthetase deficiency.
The typical presentation of holocarboxylase synthetase deficiency is seen in the neonatal period with onset occurring within hours to weeks of birth. The classic symptoms of holocarboxylase synthetase deficiency are hypotonia, lethargy, seizures, metabolic acidosis, vomiting, hyperammonemia, developmental delay, skin rash, and alopecia.
Standard newborn screening tests include detection of holocarboxylase synthetase deficiency by analysis of blood for the presence of elevated O-(3-hydroxyvaleryl)-L-carnitine. Urine organic acid analysis in holocarboxylase synthetase deficient patients will show elevated levels of lactate, 3-hydroxyisovaleric acid, 3-hydroxypropionic acid, 3-methylcrotonic acid, methylcitric acid, and tiglylglycine. Tigylglycine is an N-acylglycine formed from glycine with an amine hydrogen substituted by a 2-methylbut-2-enoyl (tiglyl) group.
Mevalonic Aciduria
Mevalonic aciduria (MVA) is an extremely rare autosomal recessive disorder caused by deficiency of mevalonate kinase (MVK), the first committed enzyme of the cholesterol biosynthesis pathway. Mevalonate is the product of the action of 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) reductase (HMGR) acting of HMG-CoA. Mevalonate is then activated by two successive phosphorylations (catalyzed by mevalonate kinase, and phosphomevalonate kinase) yielding, sequentially, mevalonate 5-phosphate and then mevalonate 5-diphosphate. The latter compound is also called 5-pyrophosphomevalonate or mevalonate 5-pyrophosphate.
In humans, mevalonate kinase is a peroxisome localized enzyme encoded by the MVK gene. The MVK gene is located on chromosome 12q24.11 and is composed of 12 exons that generate three alternatively spliced mRNAs that collectively encode two distinct protein isoforms.
The characteristic pathology of MVA is psychomotor retardation, failure to thrive, progressive cerebellar ataxia, dysmorphic features, progressive visual impairment and recurrent febrile crises. The life expectancy for MVA patients is very often compromised. Associated with the febrile episodes hepatosplenomegaly, lymphadenopathy, abdominal symptoms, arthralgia (joint pain), and skin rashes. Diagnosis of MVA is made by measurement of highly elevated levels of mevalonic acid in the urine.
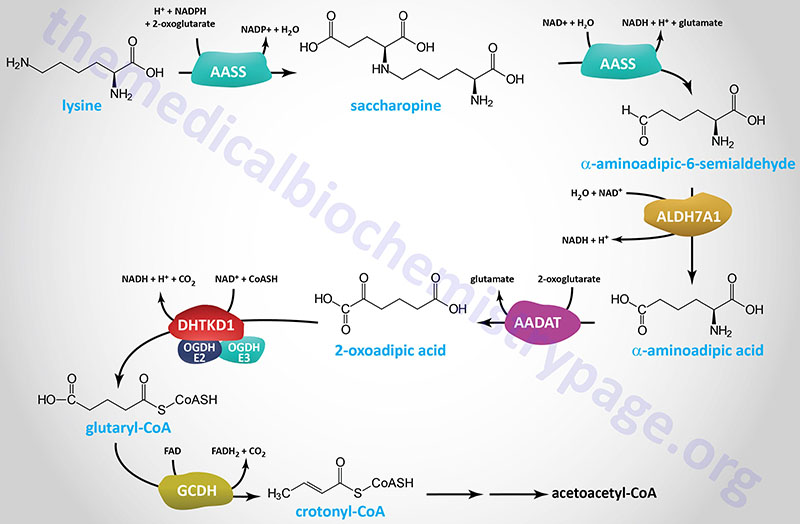
2-Ketoadipic Aciduria
The formation of 2-ketoadipic acid is formed from the oxidation of through lysine, tryptophan, and hydroxylysine. 2-Ketoadipic acid is also referred to as 2-oxoadipic acid (2-OAA) or α-ketoadipic acid. There are three major catabolic routes that produce 2-ketoadipic acid. During the oxidation of tryptophan the intermediate, 2-aminomuconate-ε-semialdehyde, is oxidized to 2-adipic acid. In the mitochondrial saccharopine pathway of lysine catabolism, 2-aminoadipic acid is oxidized to 2-ketoadipic acid. 2-Aminoadipic acid is also known as α-aminoadipic acid. In the brain specific peroxisomal pipecolic acid pathway of lysine catabolism 2-aminoadipic acid is subsequently oxidized to 2-ketoadipic acid.
2-Ketoadipic aciduria is an inherited disorder resulting from defective metabolism of 2-ketoadipic acid which leads to the accumulation and excretion of 2-ketoadipic, 2-aminoadipic, and 2-hydroxyadipic acids. Because there is accumulation of α-aminoadipic acid along with α-ketoadipic acid the disorder is also referred to as alpha-aminoadipic and alpha-ketoadipic aciduria, AAKAD. The disorder is also known as 2-aminoadipic 2-oxoadipic aciduria, AMOXAD.
The oxidation of 2-ketoadipic acid glutaryl-CoA is catalyzed by the 2-oxoadipate dehydrogenase complex. The E1 subunits of the 2-oxoadipate dehydrogenase complex are encoded by the DHTKD1 gene while the E2 and E3 subunits are shared with the 2-oxoglutarate dehydrogenase (α-ketoglutarate dehydrogenase) complex of the TCA cycle.
Mutations in the DHTKD1 gene are the primary causes of 2-ketoadipic aciduria. The DHTKD1 gene is located on chromosome 10p14 and is composed of 17 exons that encode a 919 amino acid protein.
2-Ketoadipic aciduria manifests with a wide range of clinical presentations from early-onset developmental delay, epilepsy, ataxia, and microcephaly to patients who appear completely normal.
Glutathione Synthetase Deficiency
Glutathione synthetase deficiency is a very rare autosomal recessive disorder resulting from mutations in the gene encoding one of the two enzymes, glutathione synthetase, required for the synthesis of glutathione. Glutathione (abbreviated GSH) is a tripeptide composed of glutamate, cysteine and glycine that has numerous important functions within cells. Glutathione serves as a potent reductant eliminating hydroxy radicals, peroxynitrites, and hydroperoxides; it is conjugated to drugs to make them more water soluble; it is involved in amino acid transport across cell membranes (the γ-glutamyl cycle); it is a substrate for the peptidoleukotrienes; it serves as a cofactor for some enzymatic reactions; and it serves as an aid in the rearrangement of protein disulfide bonds.
GSH is synthesized in the cytosol of all mammalian cells via the two-step reaction. The rate of GSH synthesis is dependent upon the availability of cysteine and the activity of the rate-limiting enzyme, γ-glutamylcysteine synthetase (also called glutamate-cysteine ligase, GCL). The second reaction of GSH synthesis involves the enzyme, glutathione synthetase, which condenses γ-glutamylcysteine with glycine. Both reactions of GSH synthesis require ATP.
The glutathione synthetase gene (symbol: GSS) is located on chromosome 20q11.22 and is composed of 15 exons that generate three alternatively spliced mRNAs, each of which encode the same 474 amino acid protein.
The role of GSH as a reductant is extremely important particularly in the highly oxidizing environment of the erythrocyte. The sulfhydryl of GSH can be used to reduce peroxides formed during oxygen transport. Endogenously produced hydrogen peroxide (H2O2) is reduced by GSH in the presence of selenium-dependent glutathione peroxidase. Hydrogen peroxide can also be reduced by catalase, which is present only in the peroxisomes. In the mitochondria, GSH is particularly important because mitochondria lack catalase. The resulting oxidized form of GSH consists of two molecules disulfide bonded together (abbreviated GSSG). The enzyme glutathione reductase utilizes NADPH as a cofactor to reduce GSSG back to two moles of GSH. Hence, the pentose phosphate pathway is an extremely important pathway of erythrocytes for the continuing production of the NADPH needed by glutathione reductase. In fact as much as 10% of glucose consumption, by erythrocytes, may be mediated by the pentose phosphate pathway for the production of NADPH.
Detoxification of xenobiotics or their metabolites is another major function of GSH. These compounds form conjugates with GSH either spontaneously or enzymatically in reactions catalyzed by members of the glutathione S-transferase (GST) family. The conjugates formed are usually excreted from the cell and, in the case of the liver they are excreted in the bile.
Glutathione synthetase deficiency is divided into three groups based upon clinical presentation. Mildly affected patients have
mutations affecting the stability of the enzyme, causing a compensated hemolytic anemia. Moderately affected patients experience metabolic acidosis in addition to the hemolytic anemia. Severely affected patients also develop neurological defects and show increased susceptibility to bacterial infections. Approximately 25% of GSS deficiency patients succumb to the disorder in the neonatal period as a result of bacterial infections and severe metabolic acidosis. There is currently no cure for GSS deficiency.
A characteristic organic acid accumulating in the urine of patients with GSS deficiency is 5-oxoproline which is a metabolite of glutathione. Enzymes of the ChaC family [ChaC1 (ChaC glutathione specific gamma-glutamylcyclotransferase 1)] and ChaC2 (ChaC glutathione specific gamma-glutamylcyclotransferase 2)] catabolize glutathione to 5-oxoproline and the dipeptide Cys-Gly.