Last Updated: October 30, 2025
Introduction to Dubin-Johnson Syndrome
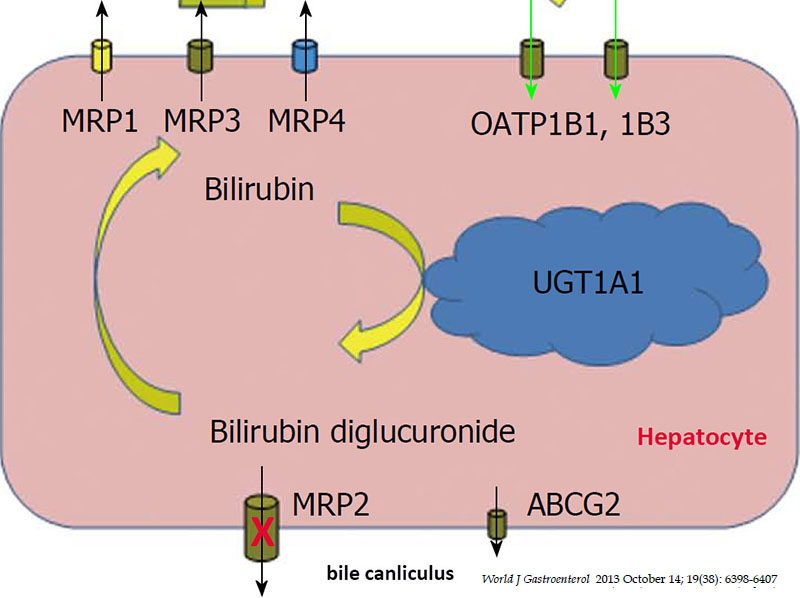
Dubin-Johnson syndrome is an autosomal recessive disorder that belongs to a family of disorders that result as a consequence of defects in the metabolism and/or excretion of bilirubin. Bilirubin is the by-product of the catabolism of heme. Normal disposition of bilirubin involves its transport to the liver where it is conjugated to the sugar molecule, glucuronic acid. This conjugation reaction converts bilirubin to a water soluble compound (bilirubin diglucuronide) that can be easily excreted in the feces.
The conjugation of bilirubin to glucuronate is catalyzed by the enzyme bilirubin-UDP-glucuronosyltransferase (bilirubin-UGT). Following the conjugation reaction bilirubin diglucuronide is transported out of hepatocytes into the bile canaliculi for transport to the gallbladder. Dubin-Johnson syndrome results from mutations in the gene encoding the bile canalicular multispecific organic anion transporter. This transporter is involved in the excretion of many non-bile organic anions by an ATP-requiring process.
Molecular Biology of Dubin-Johnson Syndrome
The canalicular multispecific organic anion transporter (CMOAT) is encoded by the ABCC2 (ATP binding cassette subfamily C member 2) gene which is a member of the ATP-binding cassette family of transporter encoding genes. The CMOAT protein has also been called the multidrug resistance-associated protein 2 gene (MRP2).
The ABCC2 gene is located on chromosome 10q24.2 spanning more than 200 kb and is comprised of 34 exons that encode a 1545 amino acid protein. Most of the mutations in the ABCC2 gene resulting in Dubin-Johnson syndrome are found in the exons encoding the cytoplasmic portion of the protein. This is the region that contains the ATP-binding cassettes.
Clinical Consequences of Hyperbilirubinemia
Excess circulation and accumulation of bilirubin (hyperbilirubinemia) results in a yellow-orange discoloration of the tissues and is most easily visible as icteric (yellowish) discoloration in the sclera of the eyes. Bilirubin toxicity (bilirubin encephalopathy) can be life threatening in neonates. Bilirubin encephalopathy is characterized by yellow discoloration of the basal ganglia in babies with intense jaundice and was first described over a century ago and the term “kernicterus” was coined to describe these physical changes. Any increase in plasma bilirubin above 20mg/dL is considered dangerous in neonates. However, individual differences in bilirubin sensitivity can result in kernicterus at lower bilirubin levels. Kernicterus occurs in infants with severe unconjugated hyperbilirubinemia and in young adults with high serum levels of unconjugated bilirubin, with the latter the result of inherited deficiencies in bilirubin-UGT.
Bilirubin has been shown to inhibit DNA synthesis, uncouple oxidative phosphorylation, and inhibit ATPase activity in brain mitochondria. Bilirubin also inhibits a variety of different classes of enzymes including dehydrogenases, electron transport proteins, hydrolases, and enzymes of RNA synthesis, protein synthesis and carbohydrate metabolism. All of these toxic effects of bilirubin are reversed by binding to albumin. In fact, albumin plays a vital role in the disposition of bilirubin in the body by keeping the compound in solution and transporting it from its sites of production (primarily bone marrow and spleen) to its site of excretion which is the liver.
Bilirubin levels are measured in the serum by an assay utilizing Ehrlich diazo reagent and results in the formation of an azobilirubin product. Conjugated bilirubin does not require addition of alcohol to promote the azotization reaction and thus, this is referred to as measurement of direct bilirubin. The reaction with unconjugated bilirubin requires the addition of alcohol and thus is referred to as the measurement of indirect bilirubin. Normal bilirubin measurements are 0.3–1.2md/dL for total (indirect + direct). Direct type bilirubin does not exist in the plasma, however, a small portion of indirect type bilirubin may present as direct reacting type and thus the serum measurement may show a direct bilirubin but this is never above 0.3mg/dL in a normal individual.
Clinical Features of Dubin-Johnson Syndrome
Dubin-Johnson syndrome is inherited as an autosomal recessive disorder characterized by mild, predominantly conjugated hyperbilirubinemia. The defect causing Dubin-Johnson syndrome leads to an abnormality in porphyrin metabolism such that more than 80% of the urinary compound from this pathway is coproporphyrin I, whereas in a normal individual it is usually less than 35%.
Due to impaired transport of epinephrine metabolites to the bile canaliculi melanin-like pigments accumulate in the liver such that there is a characteristic black appearance to the organ but with normal histology.
Jaundice is usually the only physical symptom detected in this disease. Most patients remain asymptomatic although some complain of weakness and abdominal pains. Only occasionally do patients develop hepatosplenomegaly. In many cases individuals with the disorder remain undiagnosed due to lack of obvious signs and symptoms. Women may exhibit overt symptoms for the first time when taking oral contraceptives or when pregnant.