Last Updated: October 28, 2028
Introduction to the α-Thalassemias
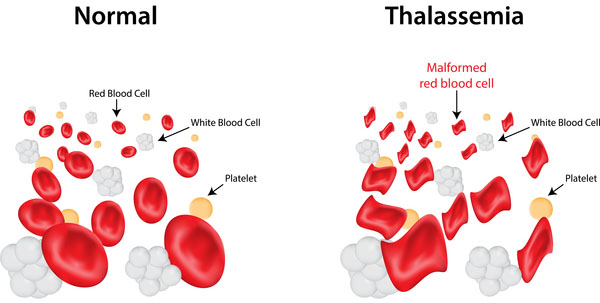
The thalassemias are the result of quantitative abnormalities in hemoglobin synthesis. With the α-thalassemias the level of α-globin production can range from none to very nearly normal levels. This is due in part to the fact that there are two identical α-globin genes on chromosome 16 in humans. Thus, the α-thalassemias involve mutations in 1 to all 4 α-globin genes.
Molecular Biology of the α-Thalassemias
The adult α-globin genes are contained within a cluster of α-globin family genes located on chromosome 16p13.3. This gene cluster spans 30 kbp in the telomere to centromere direction. The cluster is composed of the zeta (ζ; HBZ) gene, the pseudozeta (Ψζ; HBZP1) gene, the mu (μ; HBM) gene, the pseudoalpha 1 (Ψα; HBAP1) gene, the alpha 2 (α2; HBA2) gene, the alpha 1 (α1; HBA1) gene, and the theta (θ; HBQ1) gene.
The two identical adult α-globin genes (HBA1 and HBA2), as well as the other coding genes of the α-globin cluster, are composed of 3 exons that encode 142 amino acid proteins.
The zeta (ζ) globin is present in hemoglobin produced during early embryonic development is associated with the epsilon (ε) protein from the β-globin locus. This heterotetrameric hemoglobin is referred to as Hb Gower I. Later in fetal development, and in the adult, hemoglobin tetramers contain α-globin proteins produced by the HBA1 and HBA2 genes along with, predominantly, β-globin produced by the HBB gene.
Clinical Features of the α-Thalassemias
If three of the four α-globin genes are functional, individuals are completely asymptomatic. This situation is identified as the “silent carrier” state or sometimes as α-thalassemia 2. Genotypically this situation is designated αα/α– (where the dash indicates a non-functional gene) or α–/αα.
If two of the four genes are inactivated individuals are designated as “α-thalassemia trait” or as α-thalassemia 1. Genotypically this situation is designated αα/– –. The αα/– – phenotype is referred to as homozygous α0-thalassemia. In individuals of African descent with α-thalassemia 1, the disorder usually results from the inactivation of one α-globin gene on each chromosome and is genotypically designated α–/α–. This means that these individuals are homozygous for the α-thalassemia 2 chromosome. The α–/α– phenotype is referred to as homozygous α+-thalassemia.
The phenotype of α-thalassemia 1 is relatively benign. The mean red cell volume (designated MCV in clinical tests, for “mean corpuscular volume”, a red blood cell is also referred to as a corpuscle) is reduced in α-thalassemia 1 but individuals are generally asymptomatic. Normal MCV is around 90 ± 5 femtoliters (fl) and in α-thalassemia trait it is usually found to be around 81 ± 7fl. In addition, the mean corpuscular hemoglobin content (MCH) is reduced. Normal MCH is around 30 ± 2 picograms (pg). and in α-thalassemia trait it is around 26 ± 2pg.
The clinical situation becomes more severe if only one of the four α-globin genes is functional. Because of the dramatic reduction in α-globin chain production in this latter situation, a high level of β4 tetramer is present. In the adults the presence of β4 tetramers is clinically referred to as hemoglobin H disease (HbH). Afflicted individuals have moderate to marked anemia and their MCV is quite low, but the disease is not fatal. In HbH disease individuals have MCV of 65 ± 7fl and MCH of 19 ± 2pg.
The most severe situation results when no α-globin chains are made (genotypically designated: – –/– –). This leads to prenatal lethality or early neonatal death. The predominant fetal hemoglobin in afflicted individuals is a tetramer of γ-chains and is referred to as hemoglobin Bart’s. This tetrameric form of hemoglobin has very high affinity for oxygen resulting in poor oxygen release and thus, oxygen starvation in the fetal tissues. Heart failure results as the heart tries to pump more oxygenated blood to oxygen starved tissues leading to marked edema. This latter situation is called hydrops fetalis.
There are two rare disorders that are associated with α-thalassemia. One is identified as α-thalassemia-intellectual disability syndrome linked to chromosome 16 (ATR-16) and the other is identified as α-thalassemia X-linked intellectual disability syndrome (ATR-X).
As the name of ATR-16 implies this is a disorder that is the result of large deletion of the p arm of chromosome 16 that involves not only the α-globin genes but several additional genes that lie in the same general region of the p arm of chromosome 16. ATR-16 is associated microcytic hypochromic anemia typical of α-thalassemia but the disorder is also associated with a variable clinical phenotype that is characterized by mild to moderate intellectual disabilities, developmental delay, and a wide range of less characteristic dysmorphic features.
Laboratory Finding in α-Thalassemia
The various genotypes of α-thalassemia resulting from two mutant alleles, out of the four possible, are associated with decreases in the hematological values for red blood cell volume, red blood cell counts, red blood cell hemoglobin, and HbA2. Red blood cell volume is measured in femtoliters (fL) and is termed the mean corpuscular volume, MCV. Normal MCV values are in the range of 82–98 fL whereas in α-thalassemia the MCV value is indicative of microcytic anemia being <80 fL. Red blood cell hemoglobin on a per cell basis is assessed as mean corpuscular hemoglobin (MCH) which is normally 26–34 picograms (pg). In α-thalassemia the MCH value is always <26 pg. Red blood cell hemoglobin is measured g/dL where the normal range is between 12 and 16.5 gm/dL depending upon sex. In α-thalassemia the amount of hemoglobin is often below the normal range but not below 7g/dL. The normal HbA1 level is around 95% of total types of hemoglobin in the post-natal red blood cell, where around 4–5% is HbA2 (consists of the δ-globin protein) and from to 0.5%–2% is HbF (fetal hemoglobin). In α-thalassemia the amount of HbA1 is usually <3.5%. Red blood cell counts are often increased in α-thalassemia.
Laboratory Values Associated with α-Thalassemia
| Lab Value | Normal | α-Thalassemia 1 (minor) |
| MCV (fL) | 82–98 | <80 |
| MCH (pg) | 26–34 | <26 |
| Hemoglobin (g/dL) | 12–16.5 | 7–10 |
| HbA1 (%) | 95 | 90–95 |
| HbA2 (%) | 2–3 | 1.5–2.5 |
| HbF (%) | 0.5–2 | 19–50 |
| HbS (%) | 0 | 0 |
Disorders Associated with α-Thalassemia
Alpha-Thalassemia X-linked intellectual disability syndrome (ATR-X) is a syndrome that is characterized by severe intellectual impairment along with dysmorphic features, severe psychomotor impairment, hypertelorism, developmental abnormalities in genital and/or urogenital areas, along with facial dysmorphism that includes a flat nasal bridge, a triangular upturned nose, and a wide mouth. ATR-X results from point mutations in the X-linked gene identified as ATRX. The ATRX encoded protein belongs to a family of helicase/adenosine triphosphatases. The precise molecular relationship between ATRX mutations and the manifestation of symptoms of α-thalassemia such as HbH inclusions remains unclear, and not all ATR-X syndrome patients will manifest with HbH inclusions.